What Is Alagille Syndrome?
Alagille syndrome is a rare, life-threatening multisystem disease that often presents in childhood.2 With Alagille syndrome, bile ducts are abnormally narrow, malformed, and reduced in number, which leads to toxic accumulation of bile acids in the liver and, ultimately, progressive liver disease.1,3
For more information about cholestatic liver disease, visit these Resources.
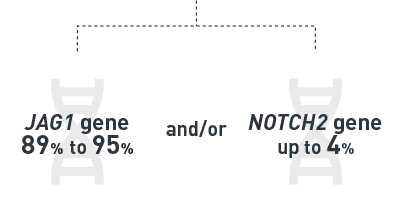
Alagille syndrome is an autosomal dominant disorder caused by mutations/deletions in the1,2,4,5:
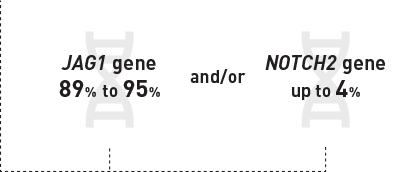
Disruptions in these genes cause defective bile duct morphogenesis and impaired angiogenesis, and abnormalities in skeletal, ocular, cardiovascular, and kidney development.6 Although 30% to 50% of individuals have an inherited pathogenic variant, the mutation occurs de novo in 50% to 70% of cases.7
Mirum is proud to sponsor free genetic testing through Travere Therapeutics to help with early diagnosis.
Alagille syndrome affects males and
females equally8

The estimated incidence of Alagille syndrome is 1 in every 30,000 to 45,000 individuals8

an estimated
2500 children
living with Alagille syndrome in
the United States9
In patients with Alagille syndrome, multiple organs/areas may be affected, including8:


Importantly, the bile duct paucity associated with Alagille syndrome leads to impaired bile flow, accumulation of bile acids in the liver and bloodstream, and cholestatic liver injury.1,10 Increased serum bile acids (sBA) lead to debilitating pruritus. This, in turn, can cause severe sleep deprivation, resulting in fatigue, a failure to thrive, and a dramatic reduction in quality of life.11,12 In approximately 15% of patients, progressive liver disease results in cirrhosis of the liver and liver failure.8 Phenotype is not a clear predictor for risk of progressive liver disease in Alagille syndrome.13
For more information about cholestatic liver disease, visit these Resources.